Vitamin D is a group of fat-soluble secosteroids responsible for intestinal absorption of calcium and phosphate. In humans, vitamin D is unique because it can be ingested as cholecalciferol (vitamin D3) or ergocalciferol (vitamin D2) and because the body can also synthesize it (from cholesterol) when sun exposure is adequate (hence its nickname, the "sunshine vitamin").
Although vitamin D is commonly called a vitamin, it is not actually an essential dietary vitamin in the strict sense, as it can be synthesized in adequate amounts by most mammals exposed to sunlight (cats and dogs cannot synthesize vitamin D and must receive it in their diet). An organic chemical compound (or related set of compounds) is only scientifically called a vitamin when it cannot be synthesized in sufficient quantities by an organism, and must be obtained from their diet. However, as with other compounds commonly called vitamins, vitamin D was discovered in an effort to find the dietary substance that was lacking in a disease, namely, rickets, the childhood form of osteomalacia.[1] Additionally, like other compounds called vitamins, in the developed world vitamin D is added to staple foods, such as milk, to avoid disease due to deficiency.
Measures of serum levels reflect endogenous synthesis from exposure to sunlight as well as intake from the diet, and it is believed that synthesis may contribute generally to the maintenance of adequate serum concentrations. The evidence indicates that the synthesis of vitamin D from sun exposure works in a feedback loop that prevents toxicity but, because of uncertainty about the cancer risk from sunlight, no recommendations are issued by theInstitute of Medicine, USA, for the amount of sun exposure required to meet vitamin D requirements. Accordingly, the Dietary Reference Intakes for vitamin D assume that no synthesis occurs and that all of a person's vitamin D is from their diet, although that will rarely occur in practice.
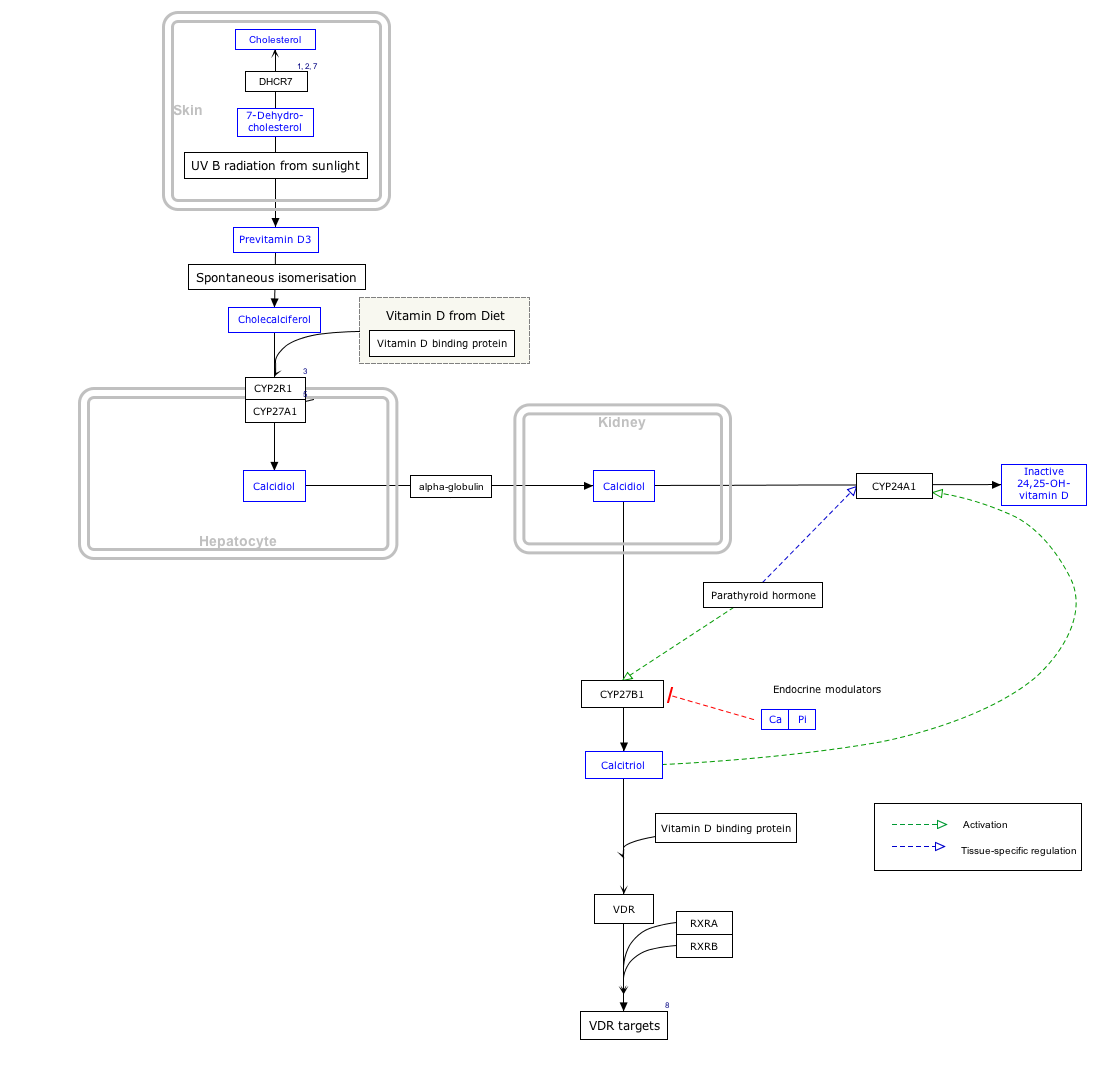
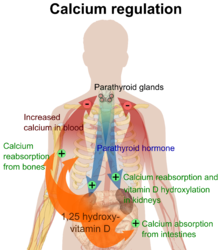
In the liver vitamin D is converted to calcidiol, which is also known as calcifediol (INN), 25-hydroxycholecalciferol, or 25-hydroxyvitamin D—abbreviated 25(OH)D; and which is the specific vitamin D metabolite that is measured in serum to determine a person's vitamin D status.[2][3] Part of the calcidiol is converted by the kidneys to calcitriol, the biologically active form of vitamin D.[4] Calcitriol circulates as a hormone in the blood, regulating the concentration of calcium and phosphate in the bloodstream and promoting the healthy growth and remodeling of bone. Calcidiol is also converted to calcitriol outside of the kidneys for other purposes, such as the proliferation, differentiation and apoptosis of cells; calcitriol also affects neuromuscular function and inflammation.[5]
Beyond its use to prevent osteomalacia or rickets, the evidence for other health effects of vitamin D supplementation in the general population is inconsistent.[6][7] The best evidence of benefit is for bone health[8] and a decrease in mortality in elderly women.
Health effects of supplements
|
The effects of vitamin D supplementation on health are uncertain.[7] A United States Institute of Medicine, (IOM) report states: "Outcomes related to cancer, cardiovascular disease andhypertension, diabetes and metabolic syndrome, falls and physical performance, immune functioning and autoimmune disorders, infections, neuropsychological functioning, and preeclampsiacould not be linked reliably with calcium or vitamin D intake and were often conflicting."[8]:5 Some researchers claim the IOM was too definitive in its recommendations and made a mathematical mistake when calculating the blood level of vitamin D associated with bone health.[10] Members of the IOM panel maintain that they used a "standard procedure for dietary recommendations" and that the report is solidly based on the data. Research on vitamin D supplements, including large scale clinical trials, is continuing.[10]
[edit]Mortality
Low blood levels of vitamin D are associated with increased mortality,[11] and giving supplementary vitamin D3 to elderly women in institutional care seems to decrease the risk of death.[9] Vitamin D2, alfacalcidol, and calcitriol do not appear to be effective.[9] However, both an excess and a deficiency in vitamin D appear to cause abnormal functioning and premature aging.[12][13][14] The relationship between serum calcidiol level and all-cause mortality is parabolic,[8] Harm from vitamin D appears to occur at a lower vitamin D level in the black population than in the white population.[8]:435
[edit]Bone health
Vitamin D deficiency causes osteomalacia (called rickets when it occurs in children). Beyond that, low serum vitamin D levels have been associated with falls, and low bone mineral density.[15]
In 2012, the U.S. Preventive Services Task Force issued a draft statement recommending that there is not enough evidence to indicate that healthy postmenopausal women should use supplemental doses of calcium or vitamin D to prevent fractures.[16]
Some studies have shown that supplementation with vitamin D and calcium may improve bone mineral density slightly, as well as decreasing the risk of falls and fractures in certain groups of people, specifically those older than 65 years.[15][17] This appears to apply more to people in institutions than those living independently.[18] The quality of the evidence is, however, poor.[19] And there does not appear to be a benefit to bone health from vitamin D without sufficient calcium.[20]
[edit]Cardiovascular disease
Evidence for health effects from vitamin D supplementation for cardiovascular health is poor.[6][21][22] Moderate to high doses may reduce cardiovascular disease risk but are of questionable clinical significance.[6][23]
[edit]Multiple sclerosis
Low levels of vitamin D are associated with multiple sclerosis. Supplementation with vitamin D may have a protective effect but there are uncertainties and unanswered questions.[24][25][26] "The reasons why vitamin D deficiency is thought to be a risk factor for MS are as follows: (1) MS frequency increases with increasing latitude, which is strongly inversely correlated with duration and intensity of UVB from sunlight and vitamin D concentrations; (2) prevalence of MS is lower than expected at high latitudes in populations with high consumption of vitamin-D-rich fatty fish; and (3) MS risk seems to decrease with migration from high to low latitudes."[24] A clinical trial sponsored by Charite University in Berlin, Germany was begun in 2011, with the goal of examining the efficacy, safety and tolerability of vitamin D3 in the treatment of Multiple Sclerosis.[27][28]
[edit]Cancer
Low vitamin D levels are associated with some cancers and with worse outcomes in other cancers, but taking supplements does not appear to help people with prostate cancer.[29] Currently evidence is insufficient to support supplementation in those with cancer.[29] Results for a protective or harmful effect of vitamin D supplementation in other types of cancer are inconclusive.[7][30]
[edit]Pregnancy
Pregnant women who take an adequate amount of vitamin D during gestation, may experience positive immune effects.[31] Pregnant women throughout the world do not take the recommended dose of vitamin D, which could negatively impact the health of the mother and her fetus.[31] 4000 IU of vitamin D3 was considered a superior regimen for supplementing pregnant women.[31]
[edit]Other
Vitamin D appears to have effects on immune function.[32] It has been postulated to play a role in influenza with lack of vitamin D synthesis during the winter as one explanation for high rates of influenza infection during the winter.[33] For viral infections, other implicated factors include low relative humidities produced by indoor heating and low temperatures that favor virus spread.[34] Low levels of vitamin D appear to be a risk factor for tuberculosis,[35] and historically it was used as a treatment.[36] As of 2011, it is being investigated in controlled clinical trials.[36] Vitamin D may also play a role in HIV.[37] Although there are tentative data linking low levels of vitamin D to asthma, there is inconclusive evidence to support a beneficial effect from supplementation.[38]Accordingly, supplementation is not currently recommended for treatment or prevention of asthma.[39] Also, preliminary data is inconclusive for supplemental vitamin D in promotion of human hair growth.[40]
[edit]Deficiency
Main article: Hypovitaminosis D
A diet deficient in vitamin D causes osteomalacia (called rickets when it occurs in children), which is a softening of the bones. In the developed world, this is a rare disease.[41][42] Low blood calcidiol (25-hydroxy-vitamin D) can result from avoiding the sun.[43] Deficiency results in impaired bone mineralization and leads to bone-softening diseases[44] including:
- Rickets, a childhood disease characterized by impeded growth and deformity of the long bones, can be caused by calcium or phosphorus deficiency as well as a lack of vitamin D; today it is largely found in low-income countries in Africa, Asia or the Middle East[45] and in those with genetic disorders such as pseudovitamin D deficiency rickets.[46] Rickets was first described in 1650 by Francis Glisson who said it had first appeared about 30 years previously in the counties of Dorset and Somerset.[47] In 1857, John Snow suggested that rickets, then widespread in Britain, was being caused by the adulteration of bakers' bread with alum.[48] The role of diet in the development of rickets[49][50] was determined by Edward Mellanby between 1918–1920.[51]Nutritional rickets exists in countries with intense year-round sunlight such as Nigeria and can occur without vitamin D deficiency.[52][53] Although rickets and osteomalacia are now rare in Britain, there have been outbreaks in some immigrant communities in which osteomalacia sufferers included women with seemingly adequate daylight outdoor exposure wearing Western clothing.[54] Having darker skin and reduced exposure to sunshine did not produce rickets unless the diet deviated from a Western omnivore pattern characterized by high intakes of meat, fish and eggs, and low intakes of high-extraction cereals.[55][56][57] The dietary risk factors for rickets include abstaining from animal foods.[54][58] Vitamin D deficiency remains the main cause of rickets among young infants in most countries, because breast milk is low in vitamin D and social customs and climatic conditions can prevent adequate UVB exposure. In sunny countries such as Nigeria, South Africa, and Bangladesh, where the disease occurs among older toddlers and children, it has been attributed to low dietary calcium intakes, which are characteristic of cereal-based diets with limited access to dairy products.[57] Rickets was formerly a major public health problem among the US population; in Denver where ultraviolet rays are approximately 20% stronger than at sea level on the same latitude,[59] almost two-thirds of 500 children had mild rickets in the late 1920s.[60] An increase in the proportion of animal protein[58][61] in the 20th century American diet coupled with increased consumption of milk [62][63] fortified with relatively small quantities of vitamin D coincided with a dramatic decline in the number of rickets cases.[64]
- Osteomalacia, a bone-thinning disorder that occurs exclusively in adults, is characterized by proximal muscle weakness and bone fragility. The effects of osteomalacia are thought to contribute to chronic musculoskeletal pain,[65][66] There is no persuasive evidence of lower vitamin D levels in chronic pain sufferers.[67]
The Director General of Research and Development and Chief Scientific Adviser for the UK Department of Health and NHS said that children aged six months to five years should be given vitamin D supplements, particularly during the winter. However, vitamin D supplements are not recommended for people who get enough vitamin D from their diets and from sunlight.[68]
Some research shows that dark-skinned people living in temperate climates have lower vitamin D levels.[69][70][70] It has been suggested that dark-skinned people are less efficient at making vitamin D because melanin in the skin hinders vitamin D synthesis; however, a recent study has found novel evidence that low vitamin D levels among Africans may be due to other reasons.[71]Recent evidence implicates parathyroid hormone in adverse cardiovascular outcomes. Black women have an increase in serum PTH at a lower 25(OH)D level than white women.[72] A large scale association study of the genetic determinants of vitamin D insufficiency in Caucasians found no links to pigmentation.[73][74]
On the other hand, the uniform occurrence of low serum 25(OH)D in Indians living in India[75] and Chinese in China,[76] does not support the hypothesis that the low levels seen in the more pigmented are due to lack of synthesis from the sun at higher latitudes. The leader of the study has urged dark-skinned immigrants to take vitamin D supplements nonetheless, saying, "I see no risk, no downside, there's only a potential benefit.[77][78] "
[edit]Toxicity
For more details on this topic, see hypervitaminosis D.
In healthy adults, sustained intake of more than 1250 micrograms/day (50,000 IU) can produce overt toxicity after several months;[79] those with certain medical conditions such as primaryhyperparathyroidism[80] are far more sensitive to vitamin D and develop hypercalcemia in response to any increase in vitamin D nutrition, while maternal hypercalcemia during pregnancy may increase fetal sensitivity to effects of vitamin D and lead to a syndrome of mental retardation and facial deformities.[80][81] Pregnant or breastfeeding women should consult a doctor before taking a vitamin D supplement.The FDA advised manufacturers of liquid Vitamin D supplements that droppers accompanying these products should be clearly and accurately marked for 400 international units (IU). In addition, for products intended for infants, FDA recommends that the dropper hold no more than 400 IU.[82] For infants (birth to 12 months), the tolerable upper limit (maximum amount that can be tolerated without harm) is set at 25 micrograms/day (1000 IU). One thousand micrograms (40,000 IU) per day in infants has produced toxicity within one month.[79] After being commissioned by the Canadian and American governments, the Institute of Medicine (IOM) as of 30 November 2010, has increased the tolerable upper limit (UL) to 2500 IU per day for ages 1–3 years, 3000 IU per day for ages 4–8 years and 4000 IU per day for ages 9–71+ years (including pregnant or lactating women).[83] Vitamin D overdose causes hypercalcemia, and the main symptoms of vitamin D overdose are those of hypercalcemia: anorexia, nausea, and vomiting can occur, frequently followed by polyuria, polydipsia, weakness, insomnia, nervousness, pruritus, and, ultimately, renal failure. Proteinuria, urinary casts, azotemia, and metastatic calcification (especially in the kidneys) may develop.[79] Vitamin D toxicity is treated by discontinuing vitamin D supplementation and restricting calcium intake. Kidney damage may be irreversible. Exposure to sunlight for extended periods of time does not normally cause vitamin D toxicity.[80] Within about 20 minutes of ultraviolet exposure in light-skinned individuals (3–6 times longer for pigmented skin), the concentrations of vitamin D precursors produced in the skin reach an equilibrium, and any further vitamin D that is produced is degraded.[84][84]
Published cases of toxicity involving hypercalcemia in which the vitamin D dose and the 25-hydroxy-vitamin D levels are known all involve an intake of ≥40,000 IU (1000 μg) per day.[80]Recommending supplementation, when those supposedly in need of it are labeled healthy, has proved contentious, and doubt exists concerning long term effects of attaining and maintaining high serum 25(OH)D by supplementation.[85]
[edit]Forms
| Name | Chemical composition | Structure |
|---|---|---|
| Vitamin D1 | molecular compound of ergocalciferol withlumisterol, 1:1 | |
| Vitamin D2 | ergocalciferol (made from ergosterol) |  |
| Vitamin D3 | cholecalciferol (made from 7-dehydrocholesterolin the skin). |  |
| Vitamin D4 | 22-dihydroergocalciferol |  |
| Vitamin D5 | sitocalciferol (made from 7-dehydrositosterol) |  |
Several forms (vitamers) of vitamin D exist (see table). The two major forms are vitamin D2 or ergocalciferol, and vitamin D3 or cholecalciferol; vitamin D without a subscript refers to either D2 or D3 or both. These are known collectively as calciferol.[86] Vitamin D2 was chemically characterized in 1932. In 1936, the chemical structure of vitamin D3 was established and proven to result from the ultraviolet irradiation of 7-dehydrocholesterol.[87]
Chemically, the various forms of vitamin D are secosteroids; i.e., steroids in which one of the bonds in the steroid rings is broken.[88] The structural difference between vitamin D2 and vitamin D3 is in their side chains. The side chain of D2 contains a double bond between carbons 22 and 23, and a methyl group on carbon 24.
Vitamin D3 (cholecalciferol) is produced by ultraviolet irradiation (UV) of its precursor 7-dehydrocholesterol. This molecule occurs naturally in the skin of animals and in milk. Vitamin D3 can be made by exposure of the skin to UV, or by exposing milk directly to UV (one commercial method).
Vitamin D2 is a derivative of ergosterol, a membrane sterol named for the ergot fungus, which is produced by some kinds of phytoplankton, invertebrates, yeasts, and higher fungi such as mushrooms. The vitaminergocalciferol (D2) is produced in all of these organisms from ergosterol, in response to UV irradiation. Like all forms of vitamin D, it cannot be produced without UV irradiation. D2 is not produced by green land plants orvertebrates, because they lack the precursor ergosterol.[89] The biological fate for producing 25(OH)D from vitamin D2 is expected to be the same as for 25(OH)D3,[90] although some controversy exists over whether or not D2 can fully substitute for vitamin D3 in the human diet.[91] [92]
[edit]Photosynthesis of vitamin D in primitive species.
Photosynthesis of vitamin D in the ocean by phytoplankton (such as coccolithophore and Emiliania huxleyi) has existed for more than 500 million years and continues to the present. Although primitive vertebrates in the ocean could absorb calcium from the ocean into their skeletons and eat plankton rich in vitamin D, land animals required another way to satisfy their vitamin D requirement for a calcified skeleton without relying on plants. Land vertebrates have been making their own vitamin D for more than 350 million years.[93]
Vitamin D can be synthesized only via a photochemical process, so land vertebrates had to ingest foods that contained vitamin D or had to be exposed to sunlight to photosynthesize vitamin D in their skin to satisfy their body's vitamin D requirement.[94]
[edit]Production in the skin
Vitamin D3 (cholecalciferol) is produced photochemically in the skin from 7-dehydrocholesterol. 7-Dehydrocholesterol is produced in relatively large quantities, 10,000 to 20,000 IU of vitamin D are produced in 30 minutes of whole-body exposure,[95] in the skin of most vertebrate animals, including humans.[96] 7-dehydrocholesterol reacts with ultraviolet light of UVB type at wavelengths between 270 and 300 nm, with peak synthesis occurring between 295 and 297 nm.[97] These wavelengths are present in sunlight when the UV index is greater than three, as well as in the light emitted by the UV lamps in tanning beds (which produce ultraviolet primarily in the UVA spectrum, but typically produce 4% to 10% of the total UV emissions as UVB). At a UV index greater than three, which occurs daily within the tropics, daily during the spring and summer seasons in temperate regions, and almost never within the arctic circles, vitamin D3 can be made in the skin.
Depending on the intensity of UVB rays and the minutes of exposure, an equilibrium can develop in the skin, and vitamin D degrades as fast as it is generated.[84]
The skin consists of two primary layers: the inner layer called the dermis, composed largely of connective tissue, and the outer, thinner epidermis. Thick epidermis in the soles and palms consists of five strata; from outer to inner they are: the stratum corneum, stratum lucidum, stratum granulosum,stratum spinosum, and stratum basale. Vitamin D is produced in the two innermost strata, the stratum basale and stratum spinosum.
The naked mole rat appears to be naturally cholecalciferol deficient, as serum 25-OH vitamin D levels are undetectable.[98] In some animals, the presence of fur or feathers blocks the UV rays from reaching the skin. In birds and fur-bearing mammals, vitamin D is generated from the oily secretions of the skin deposited onto the feathers or fur and is obtained orally during grooming.[99]
[edit]Interactive metabolism and pathway map
Click on genes, proteins and metabolites below to link to respective articles. [100]
[edit]Sunscreen
Sunscreen absorbs ultraviolet light and prevents it from reaching the skin. It has been reported that sunscreen with a sun protection factor (SPF) of 8 based on the UVB spectrum can decrease vitamin D synthetic capacity by 95 percent, whereas sunscreen with an SPF of 15 can reduce synthetic capacity by 98 percent (Matsuoka et al., 1987).[101]
[edit]Mechanism of action
Vitamin D is carried in the bloodstream to the liver, where it is converted into the prohormone calcidiol. Circulating calcidiol may then be converted intocalcitriol, the biologically active form of vitamin D, either in the kidneys or by monocyte-macrophages in the immune system. When synthesized by monocyte-macrophages, calcitriol acts locally as a cytokine, defending the body against microbial invaders.[103] Following the final converting step in the kidney, calcitriol (the physiologically active form of vitamin D) is released into the circulation. By binding to vitamin D-binding protein (VDBP), a carrier protein in the plasma, calcitriol is transported to various target organs.[88]
Calcitriol mediates its biological effects by binding to the vitamin D receptor (VDR), which is principally located in the nuclei of target cells.[88] The binding of calcitriol to the VDR allows the VDR to act as a transcription factor that modulates the gene expression of transport proteins (such as TRPV6and calbindin), which are involved in calcium absorption in the intestine.[104]
The vitamin D receptor belongs to the nuclear receptor superfamily of steroid/thyroid hormone receptors, and VDRs are expressed by cells in mostorgans, including the brain, heart, skin, gonads, prostate, and breast. VDR activation in the intestine, bone, kidney, and parathyroid gland cells leads to the maintenance of calcium and phosphorus levels in the blood (with the assistance of parathyroid hormone and calcitonin) and to the maintenance ofbone content.[64]
Vitamin D increases expression of the tyrosine hydroxylase gene in adrenal medullary cells. It also is involved in the biosynthesis of neurotrophic factors, synthesis of nitric oxide synthase, and increased glutathione levels.[105]
The VDR is known to be involved in cell proliferation and differentiation. Vitamin D also affects the immune system, and VDRs are expressed in severalwhite blood cells, including monocytes and activated T and B cells.[106]
Apart from VDR activation, various alternative mechanisms of action are known. An important one of these is its role as a natural inhibitor of signal transduction by hedgehog (a hormone involved in morphogenesis).[107][108]
One of the most important roles of vitamin D is to maintain skeletal calcium balance by promoting calcium absorption in the intestines, promoting bone resorption by increasing osteoclast number, maintaining calcium and phosphate levels for bone formation, and allowing proper functioning of parathyroid hormone to maintain serum calcium levels. Vitamin D deficiency can result in lowerbone mineral density and an increased risk of reduced bone density (osteoporosis) or bone fracture because a lack of vitamin D alters mineral metabolism in the body.[109] Thus, although it may initially appear paradoxical, vitamin D is critical for proper bone formation despite its role as a potent stimulator of bone resorption.[110]
[edit]Recommendations
[edit]Dietary reference intakes
Different institutions propose different recommendations concerning daily amounts of the vitamin.
Commonly recommended daily intake of vitamin D is not sufficient if sunlight exposure is limited.[111]
[edit]Australia and New Zealand
About a third of Australians have vitamin D deficiency.[113] Australia and New Zealand have established average intakes for vitamin D, as follows:[114] children 5.0 μg /day; adults 19–50 yr 5.0 μg/day, 51–70 yr 10.0 μg/day, >70 yr 15.0 μg/day.
[edit]Canada
According to Health Canada[115] the recommended dietary allowances (RDA) for vitamin D are:
| Age group | RDA | Tolerable Upper Intake |
|---|---|---|
| Infants 0–6 months | 400 IU* | 1000 IU |
| Infants 7–12 months | 400 IU* | 1500 IU |
| Children 1–3 years | 600 IU | 2500 IU |
| Children 4–8 years | 600 IU | 3000 IU |
| Children and Adults 9–70 years | 600 IU | 4000 IU |
| Adults > 70 years | 800 IU | 4000 IU |
| Pregnancy & Lactation | 600 IU | 4000 IU |
Note*: Adequate Intake rather than Recommended Dietary Allowance.
[edit]European Union
The recommended daily amount for vitamin D in the European Union is 5 µg.[116]
The European Menopause and Andropause Society (EMAS) recommended 15 µg (600 IU) until age 70, and 20 µg (800 IU) in older than 71 years, in postmenopausal women. This dose should be increased up to 4,000 IU/day in some patients with very low vitamin D status or in case of co-morbid conditions.[117]
According to the European Food Safety Authority the Tolerable Upper Intake Levels[118] are:
- 0-12 months: 25 µg/day (1000 IU)
- 1-10 years: 50 µg/day (2000 IU)
- 11-17 years: 100 µg/day (4000 IU)
- 17+: 100 µg/day (4,000 IU)
- Pregnant/lactating women: 100 µg/day (4,000 IU)
[edit]United States
According to the United States Institute of Medicine,[8] the recommended dietary allowances of vitamin D are:
- 1–70 years of age: 600 IU/day (15 μg/day)
- 71+ years of age: 800 IU/day (20 μg/day)
- Pregnant/lactating: 600 IU/day (15 μg/day)
[edit]Upper intake levels
The Tolerable Upper Intake Level is defined as "the highest average daily intake of a nutrient that is likely to pose no risk of adverse health effects for nearly all persons in the general population.[8]:403 " Although tolerable upper intake levels are believed to be safe, information on the long-term effects is incomplete and these levels of intake are not recommended:[8]:403:433
- 0–6 months of age: 1,000 IU (25 µg/day)
- 6–12 months of age: 1,500 IU (37.5 µg/day)
- 1–3 years of age: 2,500 IU (62.5 µg/day)
- 4–8 years of age: 3,000 IU (75 µg/day)
- 9–71+ years of age: 4,000 IU (100 µg/day)
- Pregnant/lactating: 4,000 IU[8]:5(100 µg/day)
[edit]Comment
The Dietary Reference Intake for vitamin D issued by the American (U.S.) Institute of Medicine (IOM) in 2010 superseded a previous recommendation which had Adequate Intake status. The recommendations were formed assuming the individual has no skin synthesis of vitamin D because of inadequate sun exposure. The reference intake for vitamin D refers to total intake from food, beverages and supplements, is intended for the North American population, and assumes that calcium requirements are being met.[8]:5
One school of thought contends that human physiology is fine tuned to an intake of 4000–12,000 IU/day from sun exposure with concomitant serum 25-hydroxyvitamin D levels of 40 to 80 ng/mL[119] and that this is required for optimal health. Proponents of this view, who include some members of the panel that drafted a now superseded 1997 report on vitamin D from the Institute of Medicine, contend that the IOM's warning about serum concentrations above 50 ng/mL lacks biological plausibility. They suggest that for some people reducing the risk of preventable disease requires a higher level of vitamin D than that recommended by the IOM.[120][119]
[edit]Serum 25-hydroxyvitamin D
US labs generally report 25(OH)D levels as ng/mL. Other countries often use nmol/L.
A U.S. Institute of Medicine committee concluded that a serum 25-hydroxyvitamin D level of 20 ng/mL (50 nmol/L) is desirable for bone and overall health. The Dietary Reference Intakes for vitamin D are chosen with a margin of safety and 'overshoot' the targeted serum value to ensure that the specified levels of intake achieve the desired serum 25-hydroxyvitamin D levels in almost all persons. It is assumed there are no contributions to serum 25-hydroxyvitamin D level from sun exposure and the recommendations are fully applicable to people with dark skin or negligible exposure to sunlight.:1
The Institute found that serum 25-hydroxyvitamin D concentrations above 30 ng/mL (75 nmol/L) are "not consistently associated with increased benefit". Serum 25-hydroxyvitamin D levels above 50 ng/mL (125 nmol/L) may be cause for concern.[8]
There is a lower risk of cardiovascular disease when vitamin D ranged from 20 to 60 nmol/L (8 to 24 ng/mL). There appears to be a "threshold effect" once 60 nmol/L (24 ng/mL) have been reached i.e., levels of vitamin D over 60 nmol/L did not show added benefit.[121]
[edit]Allowable health claims
Apart from the above discussion on health effects or scientific evidence for lowering disease risk, governmental regulatory agencies stipulate for the food industry health claims allowable as statements on packaging.
- normal function of the immune system
- normal inflammatory response
- normal muscle function
- reduced risk of falling in people over age 60[123]
US Food and Drug Administration (FDA)
- may reduce the risk of osteoporosis[124]
- adequate calcium and regular exercise may help to achieve strong bones in children and adolescents and may reduce the risk of osteoporosis in older adults. An adequate intake of vitamin D is also necessary[125]
[edit]Dietary sources
[edit]Vitamin D2
Main article: Ergocalciferol
- Mushrooms, portabella, exposed to ultraviolet light, raw: Vitamin D2: 11.2 μg (446 IU)
- Mushrooms, portabella, exposed to ultraviolet light, grilled: Vitamin D2: 13.1 μg (524 IU)
- Mushrooms, shiitake, dried: Vitamin D2: 3.9 μg (154 IU)
- Mushrooms, shiitake, raw: Vitamin D2: 0.4 μg (18 IU)
- Mushrooms, portabella, raw: Vitamin D2: 0.3 μg (10 IU)
- Mushroom powder, any species, illuminated with sunlight or artificial ultraviolet light sources
Vitamin D2, or ergocalciferol found in fungi, is synthesized from viosterol, which in turn is activated when ultraviolet light stimulates ergosterol.[129]
Human bioavailability of vitamin D2 from vitamin D2-enhanced button mushrooms via UV-B irradiation is effective in improving vitamin D status and not different from a vitamin D2 supplement.[130]from UV-irradiated yeast baked into bread is bioavailable.[131] By visual assessment or using a chromometer, no significant discoloration of irradiated mushrooms, as measured by the degree of "whiteness", was observed.[132] Claims have been made that a normal serving (approx. 3 oz or 1/2 cup, or 60 grams) of fresh mushrooms treated with ultraviolet light have increased vitamin D content to levels up to 80 micrograms,[133] or 2700 IU if exposed to just 5 minutes of UV light after being harvested.[134]
- Alfalfa (Medicago sativa subsp. sativa), shoot: 4.8 μg (192 IU) vitamin D2, 0.1 μg (4 IU) vitamin D3 (per 100 g).[135]
- Cladina arbuscula specimens grown under different natural conditions: The contents of vitamin D3 range from 0.67 to 2.04 μg g⁻¹ dry matter in the thalli of C. arbuscula specimens grown under different natural conditions, while provitamin D3 could not be detected. The ranges for provitamin D2 and vitamin D2 were 89-146 and 0.22-0.55 μg g⁻¹ dry matter, respectively, while the contents of provitamin D3 were below the detection limit (0.01 microg g(-1) dry matter).[136]
[edit]Vitamin D3
Main article: Cholecalciferol
In some countries, staple foods are artificially fortified with vitamin D.[137]
- Animal sources [5]
- Fish liver oils, such as cod liver oil, 1 Tbs. (15 ml) provides 1360 IU (90.6 IU/ml)
- Fatty fish species, such as:
- Catfish (wild), 85 g (3 oz) provides 425 IU (5 IU/g)
- Salmon, cooked, 100 g (3.5 oz) provides 360 IU (3.6 IU/g)
- Mackerel, cooked, 100 g (3.5 oz), 345 IU (3.45 IU/g)
- Sardines, canned in oil, drained, 50 g (1.75 oz), 250 IU (5 IU/g)
- Tuna, canned in oil, 100 g (3.5 oz), 235 IU (2.35 IU/g)
- Eel, cooked, 100 g (3.5 oz), 200 IU (2.00 IU/g)
- A whole egg provides 20 IU if egg weighs 60 g (0.333 IU/g)
- Beef liver, cooked, 100 g (3.5 oz), provides 15 IU (0.15 IU/g)
[edit]History
American researchers Elmer McCollum and Marguerite Davis in 1913 discovered a substance in cod liver oil which later was called "vitamin A". British doctor Edward Mellanby noticed dogs that were fed cod liver oil did not develop rickets and concluded vitamin A, or a closely associated factor, could prevent the disease. In 1921, Elmer McCollum tested modified cod liver oil in which the vitamin A had been destroyed. The modified oil cured the sick dogs, so McCollum concluded the factor in cod liver oil which cured rickets was distinct from vitamin A. He called it vitamin D because it was the fourth vitamin to be named.[138][139][140] It was not initially realized that, unlike other vitamins, vitamin D can be synthesised by humans through exposure to UV light.
In 1923, it was established that when 7-dehydrocholesterol is irradiated with light, a form of a fat-soluble vitamin is produced (now known as D3). Alfred Fabian Hess showed "light equals vitamin D."[141] Adolf Windaus, at the University of Göttingen in Germany, received the Nobel Prize in Chemistry in 1928, for his work on the constitution of sterols and their connection with vitamins.[142]In 1929 a group at NIMR in Hampstead, London, were working on the structure of vitamin D, which was still unknown, as well as the structure of steroids. A meeting took place with J.B.S. Haldane, J.D. Bernal and Dorothy Crowfoot to discuss possible structures, which contributed to bringing a team together. X-ray crystallography demonstrated that sterol molecules were flat, not as proposed by the German team led by Windaus. In 1932 Otto Rosenheim and Harold King published a paper putting forward structures for sterols and bile acids which found immediate acceptance.[143] The informal academic collaboration between the team members Robert Benedict Bourdillon, Otto Rosenheim (mentioned above), Harold King (mentioned above) and Kenneth Callow was very productive and led to the isolation and characterization of vitamin D.[144] At this time the policy of the Medical Research Council was not to patent discoveries, believing that results of medical research should be open to everybody. In the 1930s Windaus clarified further the chemical structure of vitamin D.[145]
In 1923, American biochemist Harry Steenbock at the University of Wisconsin demonstrated that irradiation by ultraviolet light increased the vitamin D content of foods and other organic materials.[146] After irradiating rodent food, Steenbock discovered the rodents were cured of rickets. A vitamin D deficiency is a known cause of rickets. Using $300 of his own money, Steenbock patented his invention. His irradiation technique was used for foodstuffs, most memorably for milk. By the expiration of his patent in 1945, rickets had been all but eliminated in the US.[147]
In 1971-72 the further metabolism of vitamin D to active forms was discovered. In the liver vitamin D was found to be converted to calcidiol[148][149] Part of the calcidiol is then converted by the kidneys to calcitriol, the biologically active form of vitamin D.[4] Calcitriol circulates as a hormone in the blood, regulating the concentration of calcium and phosphate in the bloodstream and promoting the healthy growth and remodeling of bone. Both calcidiol and calcitriol were identified by a team led by Michael F. Holick.[150][4]
[edit]Industrial production
Vitamin D3 (cholecalciferol) is produced industrially by exposing 7-dehydrocholesterol to UVB light, followed by purification.[151] The 7-dehydrocholesterol is a natural substance in wool grease (lanolin) from sheep or other woolly animals. Vitamin D2 (ergocalciferol) is produced in a similar way using ergosterol from yeast or mushrooms as a starting material.[151]
This article taken from Wikipedia (http://en.wikipedia.org/wiki/Vitamin_D)


No comments:
Post a Comment